| Case Report | ||
J. Microbiol. Infect. Dis., (2024), Vol. 14(2): 88–92 Case Report Case series of calcaneal Osteomyelitis in patients with MelioidosisKarthik Babu Raj*, Neeraj Kotteppattu Chandran, Manojan ThekkedathDepartment of Internal Medicine, Malabar Institute of Medical Science, Nilambur, India *Corresponding Author: Karthik Babu Raj, Department of Internal Medicine, Malabar Institute of Medical Science, Nilambur, India. Email: k4karthik007 [at] gmail.com Submitted: 14/03/2024 Accepted: 04/05/2024 Published: 30/06/2024 © 2024 Journal of Microbiology and Infectious Diseases
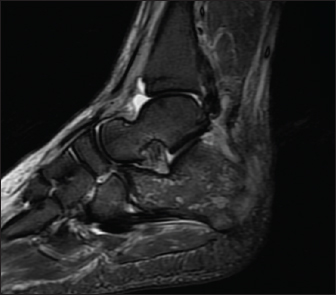
ABSTRACTBackground: Melioidosis is an emerging infectious disease caused by the Gram-negative bacterium Burkholderia pseudomallei, which can lead to a range of clinical manifestations including acute septicaemia and chronic localized infections. Osteomyelitis is an uncommon but well-recognized complication of melioidosis, with the calcaneus being a relatively rare site of involvement. Case Description: The authors present a case series of three patients with calcaneal osteomyelitis caused by Burkholderia pseudomallei, infection. All three patients presented with non-specific symptoms like fever and weight loss, followed by localized ankle/foot pain and swelling. Diagnosis was made based on imaging findings (radiographs and MRI) and isolation of Burkholderia pseudomallei, from blood or pus cultures. Treatment involved a combination of initial intravenous antibiotic therapy (meropenem or ceftazidime) for 4–6 weeks, followed by oral trimethoprim-sulfamethoxazole for 6 months. One patient required surgical drainage of a plantar abscess. All patients had a favorable clinical outcome with a resolution of osteomyelitis on follow-up imaging. Conclusion: Calcaneal osteomyelitis is a rare but potentially serious complication of melioidosis. Early recognition and prompt initiation of appropriate antibiotic therapy are crucial for favorable outcomes. Clinicians should maintain a high index of suspicion for osteomyelitis in patients with melioidosis, especially in patients from Endemic areas as well as in patients with risk factors like diabetes. Close follow-up and monitoring for potential relapse or reactivation are essential, particularly in immunocompromised individuals.Keywords: Melioidosis, Burkholderia pseudomallei, Osteomyelitis, Calcaneal, Case series. IntroductionMelioidosis is an emerging infectious disease caused by the Gram-negative bacterium Burkholderia pseudomallei, found in soil and water in tropical and subtropical regions (Wiersinga et al., 2012). The clinical manifestations range from acute septicaemia to chronic localized infections, with a high mortality rate in untreated cases (Limmathurotsakul et al., 2022). Osteomyelitis is an uncommon but well-recognized complication of melioidosis, occurring in approximately 3.8% of cases (Currie et al., 2010). While any bone can be affected, calcaneal osteomyelitis is relatively rare, with only a few cases reported in the literature (Chetchotisakd et al., 2008; Dance, 2014). Here, we present a case series of three patients with calcaneal osteomyelitis caused by B. pseudomallei infection, highlighting the clinical presentation, diagnosis, and management of this unusual complication. Case DetailsPatient 1A 70-year-old male known to have diabetes mellitus presented with a 1 month history of fever and weight loss. History of multiple hospital visits and several courses of oral and intravenous antibiotics were present. Physical examination revealed hepatosplenomegaly. As he was fitting the criteria for Pyrexia of Unknown origin, work for the same was done. Routine investigations showed neutrophilic leucocytosis with raised inflammatory markers. Widal was negative. Ultrasound abdomen showed features of chronic liver disease. Contrast CT scan of abdomen showed splenic infarcts. He was started on antibiotics, but he had ongoing fever spikes. While in hospital he developed difficulty in walking due to left ankle pain. MRI foot (Fig. 1) was taken showed small intraosseous abscess in calcaneal bone. Blood cultures grew B. pseudomallei. The patient had a good recovery and was followed up in the outpatient clinic ray foot (Fig. 2) was repeated showed a resolution of osteomyelitis. Patient 257-year-old male with diabetes, presented with complaints of intermittent fever for 4 weeks. It was associated with loss of appetite and significant loss of weight. No associated pain abdomen, vomiting, altered bowel and bladder habits. On physical examination, he had hepatomegaly. Workup for pyrexia of unknown origin was done. Mantoux test was negative. Chest X-ray showed prominent Broncho vascular markings. Contrast CT of abdomen showed splenic infarct with intraluminal short segment partial thrombosis of the proximal splenic vein along with heterogeneously enhancing subcarinal and right lower paratracheal mediastinal lymph nodes with central necrosis — probably granulomatous infection. Endobronchial ultrasound guided fine needle aspiration biopsy of mediastinal lymph nodes was done. Cytology was negative for malignancy. Histopathological report was suggestive of acute suppurative inflammation, with negative gram stain and Acid-Fast stains. But his blood culture grew B. pseudomallei and the whole clinical picture was suggestive of melioidosis. He also developed pain and swelling around left ankle joint while in hospital. On examination he had tenderness and warmth around left ankle with restricted movements. Orthopaedics consultation was obtained and an MRI ankle joint (Fig. 3) was done which showed features of acute osteomyelitis of calcaneum (multiple micro abscess) with adjacent intermuscular and fascial abscesses. Ultrasound guided aspiration of the plantar abscess was done and pus was aspirated. Culture grew B. Pseudomallei. The patient was diagnosed with osteomyelitis caused by melioidosis and was treated with intravenous Meropenem for 6 weeks, followed by oral cotrimoxazole for another six months. The patient had a good recovery and was followed up in the outpatient clinic.
Fig. 1. MRI Rt foot—patient 1.
Fig. 2. Xray Rt foot after 3 months of treatment—patient 1.
Fig. 3. MRI Rt. foot—patient 2.
Fig. 4. Xray foot—patient 3. Patient 3A 75-year-old male with a history of diabetes mellitus presented with a 3-week history of fever and left shoulder pain, back pain and leg pain. He reported no recent travel or exposure to known environmental sources of B. pseudomallei. Physical examination revealed erythema and tenderness over the left shoulder and tenderness over right foot and over the dorsal spine. Radiographs showed features fitting with osteomyelitis of left humerus. By the time blood cultures grew B. pseudomallei. X-ray foot (Fig. 4) taken showed osteomyelitis changes. The patient was diagnosed with osteomyelitis caused by melioidosis and was treated with intravenous ceftazidime and doxycycline for 6 months, followed by oral cotrimoxazole for another 6 months. The patient had a good recovery and was followed up in the out-patient clinic.
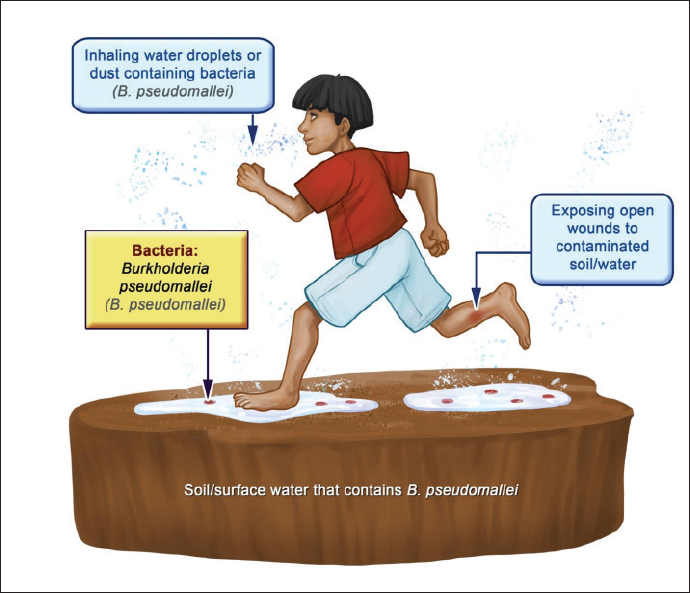
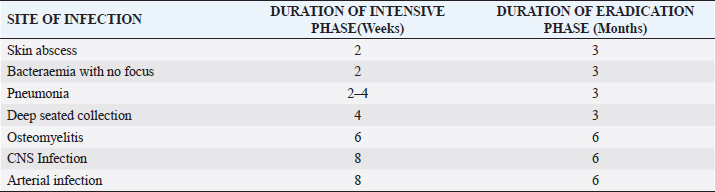
Fig. 5. Route of entry of Burkholderia pseudomallei from environment. DiscussionMelioidosis is endemic in Southeast Asia and northern Australia, with the highest incidence reported in Northeast Thailand and northern Australia (Currie et al., 2011). Risk factors for acquiring melioidosis include diabetes mellitus, excessive alcohol consumption, chronic lung disease, chronic renal disease, and immunosuppression (Currie et al., 2005). In our case series, two patients had diabetes mellitus, which is a well-established risk factor for melioidosis and its complications, including osteomyelitis (Cheah et al., 2022). The clinical manifestations of melioidosis can range from asymptomatic infection to acute fulminant sepsis, depending on the host’s immune status and the inoculum size (Kurniawan, et al., 2011). The route of entry of B. pseudomallei can be from direct percutaneous inoculation during exposure to wet season soils or contaminated water through injuries in skin or to Lungs through inhalation(Fig. 5). Osteomyelitis is a rare complication, occurring in approximately 3.8% of melioidosis cases (Currie et al., 2010). The calcaneus is an uncommon site for osteomyelitis, with only a few reported cases in the literature (Jane et al., 2012; Raja and Scarsbrook, 2016 et al). Table 1. Duration of antibiotics according to site of infection (Darwin Melioidosis Guideline).
In our case series, all three patients presented with non-specific symptoms like fever and weight loss, followed by localized ankle/foot pain and swelling. Diagnosis of calcaneal osteomyelitis was made based on imaging findings (radiographs and MRI) and isolation of Burkholderia pseudomallei, from blood or pus cultures. Early recognition of osteomyelitis is crucial, as delayed diagnosis and improper course of treatment can lead to significant morbidity and mortality (Raja, and Scarsbrook, 2016). The management of osteomyelitis caused by melioidosis involves a combination of appropriate antibiotic therapy and surgical intervention, if necessary (Jane, et al., 2012). The Infectious Diseases Society of America recommends initial intravenous therapy with ceftazidime, meropenem, or a carbapenem for at least 2 weeks, followed by oral eradication therapy with trimethoprim-sulfamethoxazole for 3–6 months (Gupta, et al., 2021). In our case series, all patients received initial intravenous antibiotic therapy (meropenem or ceftazidime) for 4–6 weeks (Table 1), followed by oral trimethoprim-sulfamethoxazole for 6 months. One patient required surgical drainage of a plantar abscess. All patients had a favourable clinical outcome with resolution of osteomyelitis on follow-up imaging. The prognosis of osteomyelitis caused by melioidosis depends on several factors, including the patient’s immune status, the presence of risk factors (e.g., diabetes), the extent of bone involvement, and the prompt initiation of appropriate antibiotic therapy (Zueter, et al., 2016). Delayed diagnosis and improper course /duration of treatment can lead to significant morbidity, including chronic osteomyelitis, bone deformities, amputation and even recurrence rarely (Guerrier G, D’Ortenzio E. 2022). In our case series, all three patients had a good clinical outcome with resolution of osteomyelitis after receiving prolonged antibiotic therapy. However, close follow-up is essential, as relapse and reactivation of melioidosis can occur, particularly in immunocompromised individuals (Rajasekaran, et al., 2022). This case series has some limitations, including the small number of cases and the retrospective nature of the study. Further research is needed to better understand the risk factors, clinical presentation, and optimal management strategies for calcaneal osteomyelitis caused by melioidosis. Additionally, larger prospective studies investigating the long-term outcomes and potential complications of this condition would be valuable. ConclusionCalcaneal osteomyelitis is a rare but potentially serious complication of melioidosis. Early recognition and prompt initiation and proper duration of appropriate antibiotic therapy are crucial for favourable outcomes. Clinicians should maintain a high index of suspicion for osteomyelitis in patients with melioidosis, especially in patients from Endemic areas as well as in patients with risk factors like diabetes, presenting with localized bone pain and swelling as the duration of treatment is the dependent on the site of involvement. Close follow-up and monitoring for potential relapse or reactivation are essential, particularly in immunocompromised individuals. AcknowledgmentThe authors would like to thank the patients for allowing their cases to be presented in this series. We also acknowledge the team (Orthopedicians, Radiologists and Physicians) at Malabar Institute of Medical Science who were involved in the care of these patients. Authors’ contributionKarthik Babu Raj and Neeraj Kottepppattu Chandran were involved in patient care, collected the data, and drafted the manuscript. Manojan Thekkedath supervised the project and critically revised the manuscript. All authors approved the final version of the manuscript. FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Conflict of interestThe authors declare no conflict of interest. Data availabilityThe data that support the findings of this case series are available from the corresponding author upon reasonable request and with permission of the institutional ethics committee. ReferencesCurrie, B.J., Ward, L. and Cheng, A.C. 2010. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year prospective melioidosis study. Trans. R. Soc. Trop. Med. Hyg. 104(11), 713–722. Currie, B.J., Jacups, S.P., Cheng, A.C., Fisher, D.A., Anstey, N.M., Huffam, S.E. and Everett, E.D. 2011. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop. Med. Int. Health 16(4), 409–529. Currie, B.J., Fisher, D.A., Anstey, N.M. and Jacups, S.P. 2005. Melioidosis: acute and chronic disease, relapse and re-activation. Trans. R. Soc. Trop. Med. Hyg. 99(2), 183-197. Chetchotisakd, P., Chierakul, W., Chaowagul, W., Anunnatsiri, S. and Nica, N.P. 2008. Melioidosis: a recurring missed diagnosis. Emerg. Infect. Dis. 14(8), 1291–1292. Cheah, B.H., Tan, P.K., Anuar, G.R., Nordin, S.A., Zaidah, A.R. and Sungap, S. 2022. Redefining melioidosis: a missed medical emergency. Med. J. Malaysia 77(2), 19–24. Dance, D.A.B. 2014. Melioidosis. Curr. Trop. Med. Rep. 1(1), 1–7. Gupta, A.R., Sharma, A., Kaul, R., Barsalohai, S., Kar, R. and Rajput, R. 2021. Cutaneous melioidosis: a rare case report from India. Indian Dermatol. Online J. 12(6), 1032–1035. Guerrier, G. and D’Ortenzio, E. 2022. Melioidosis in the Caribbean: an emerging disease? Emerg. Infect. Dis. 28(4), 881–882. Jane, L., Rajendran, N., Anuar, A.S.S. and Chan, Y.Y. 2012. A case series of melioidosis lymphadenitis and classical melioidosis. Trop. Biomed. 29(2), 259–265. Kurniawan, R.A., Kuswandi, C.M. and Mertaniasih, N.M. 2011. Melioidosis: a case series from Bali, Indonesia. Trop. Med. Surg. 19(1), 28–32. Limmathurotsakul, D., Golge, O., Dance, D.A.B., Currie, B.J. and Whatmore, A.M. 2022. Melioidosis: a review and update. Emerg. Infect. Dis. 28(4), 649–663. Raja, I.S. and Scarsbrook, A.F. 2016. Imaging of melioidosis musculoskeletal involvement. Semin. Musculoskelet. Radiol. 20(2), 137–143. Rajasekaran, S.S., Sivakumar, N. and Joe, V.M. 2022. Musculoskeletal manifestations of melioidosis: a review of imaging features. Skeletal Radiol. 51, 1159–1171 Wiersinga, W.J., Currie, B.J. and Peacock, S.J. 2012. Melioidosis. N. Engl. J. Med. 367(11), 1035–1044. Zueter, A., Yean, C.Y., Abumarzouq, M., Rahman, Z.A., Deris, Z.Z. and Harun, A. 2016. The epidemiology and clinical spectrum of melioidosis in a teaching hospital in a North-Eastern state of Malaysia: a fifteen-year review. BMC Infect. Dis. 16, 333. | ||
| How to Cite this Article |
| Pubmed Style Raj KB, Chandran NK, Thekkedath M. Case series of calcaneal osteomyelitis in patients with melioidosis. J Microbiol Infect Dis. 2024; 14(2): 88-92. doi:10.5455/JMID.2024.v14.i2.7 Web Style Raj KB, Chandran NK, Thekkedath M. Case series of calcaneal osteomyelitis in patients with melioidosis. https://www.jmidonline.org/?mno=194292 [Access: January 25, 2026]. doi:10.5455/JMID.2024.v14.i2.7 AMA (American Medical Association) Style Raj KB, Chandran NK, Thekkedath M. Case series of calcaneal osteomyelitis in patients with melioidosis. J Microbiol Infect Dis. 2024; 14(2): 88-92. doi:10.5455/JMID.2024.v14.i2.7 Vancouver/ICMJE Style Raj KB, Chandran NK, Thekkedath M. Case series of calcaneal osteomyelitis in patients with melioidosis. J Microbiol Infect Dis. (2024), [cited January 25, 2026]; 14(2): 88-92. doi:10.5455/JMID.2024.v14.i2.7 Harvard Style Raj, K. B., Chandran, . N. K. & Thekkedath, . M. (2024) Case series of calcaneal osteomyelitis in patients with melioidosis. J Microbiol Infect Dis, 14 (2), 88-92. doi:10.5455/JMID.2024.v14.i2.7 Turabian Style Raj, Karthik Babu, Neeraj Kotteppattu Chandran, and Manojan Thekkedath. 2024. Case series of calcaneal osteomyelitis in patients with melioidosis. Journal of Microbiology and Infectious Diseases, 14 (2), 88-92. doi:10.5455/JMID.2024.v14.i2.7 Chicago Style Raj, Karthik Babu, Neeraj Kotteppattu Chandran, and Manojan Thekkedath. "Case series of calcaneal osteomyelitis in patients with melioidosis." Journal of Microbiology and Infectious Diseases 14 (2024), 88-92. doi:10.5455/JMID.2024.v14.i2.7 MLA (The Modern Language Association) Style Raj, Karthik Babu, Neeraj Kotteppattu Chandran, and Manojan Thekkedath. "Case series of calcaneal osteomyelitis in patients with melioidosis." Journal of Microbiology and Infectious Diseases 14.2 (2024), 88-92. Print. doi:10.5455/JMID.2024.v14.i2.7 APA (American Psychological Association) Style Raj, K. B., Chandran, . N. K. & Thekkedath, . M. (2024) Case series of calcaneal osteomyelitis in patients with melioidosis. Journal of Microbiology and Infectious Diseases, 14 (2), 88-92. doi:10.5455/JMID.2024.v14.i2.7 |