| Research Article | ||
J Microbiol Infect Dis. 2023; 13(3): 155-164 J. Microbiol. Infect. Dis., (2023), Vol. 13(3): 155–164 Original Research Relapse and complications of brucellosis: Findings of a disease quality registryFariba Keramat1, Manochehr Karami2, Mojgan Mamani1, Ali Saadatmand1*, Seyyed Hamid Hashemi1, Mohammad Yousef Alikhani1, Saeid Bashirian3 and Zahra Shivapour41Brucellosis Research Center, Hamadan University of Medical Sciences, Hamadan, Iran 2Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran 3Department of Public Health, Social Determinants of Health Research Center, School of Health, Hamadan University of Medical Sciences, Hamadan, Iran 4Department of Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran *Corresponding Author: Ali Saadatmand. Brucellosis Research Center, Hamadan University of Medical Sciences, Hamadan, Iran. Email: ali.s_umsha [at] yahoo.com Submitted: 20/07/2022 Accepted: 12/08/2023 Published: 30/09/2023 © 2023 Journal of Microbiology and Infectious Diseases
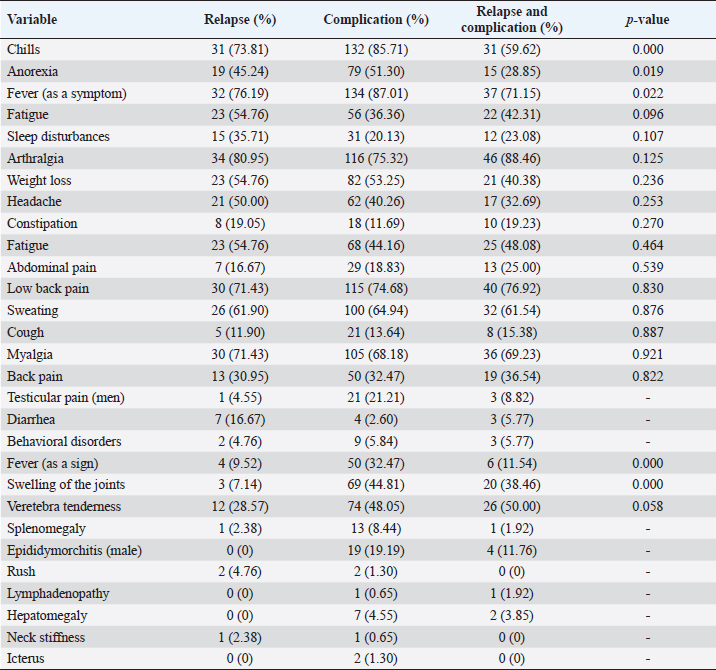
AbstractBackground: Brucellosis can be chronic or associated with relapse and complications like other chronic diseases, and a quality registry system is required. Aim: This study was designed and carried out to record the quality of relapse and complications of brucellosis in Hamadan, west of Iran. Methods: In a quality registry study, in the first phase, all patients referred to Sina Hospital and Imam Khomeini Clinic in Hamadan entered the study from September 2015 to January 2017. All information about the patients including demographic characteristics, clinical signs and symptoms, complications, and laboratory findings have been entered in the questionnaire and designed software of quality registry of relapse and complications of brucellosis. Results: A total of 248 patients with brucellosis with a mean age of 43.38 ± 17.67 (range: 13–92) years old were enrolled in the study, of which 155 patients (62.5%) were male and 80.65% of patients lived in rural areas. The most common complications were sacroiliitis 33.06% (95% CI: 27.24%, 39.29%), arthritis 29.44% (95% CI: 23.83%, 35.53%) (the most common involvement were left and right knee joints 38.36% and 35. 62%, respectively), spondylitis 22.98% (95% CI: 17.89%, 28.72%) (in lumbar vertebrae L4 and L5 were 70.18% and 68.24%, respectively), epididymorchitis (14.84%, 95% CI: 9.64%, 21.42%) in men, neurobrucellosis (3.63%, 95% CI: 1.67%, 6.77%), hepatitis (1.21%, 95% CI: 0.25%, 3.53%), and abortion in three of four pregnant women and one case of eye involvement. Conclusion: The results of this study can be used for evidence-based decision-making to diagnose and better management of relapse and complications in patients with brucellosis. Keywords: Brucellosis, Relapse, Complications, Registry, Hamadan. IntroductionBrucellosis is a common bacterial disease between humans and livestock that is transmitted through direct or indirect human contact with infected animals or contaminated dairy products. The clinical manifestations of brucellosis are wide-ranging from asymptomatic infection to complicated forms (Franc et al., 2018; Hull and Schumaker, 2018). Brucella is a Gram-negative cocobacillus and there are different types that at least four of them cause disease in humans, which are Brucella abortus, Brucella suis, Brucella melitensis, and Brucella canis (Olsen and Palmer, 2014). The clinical classification of brucellosis is subclinical, acute, subacute, chronic, and localized and Brucella involves different organs. Brucella may present with nonspecific symptoms such as fever, bone pain, muscle aches, weakness, sweating, weight loss, and headache (Hull and Schumaker, 2018; Olsen and Palmer, 2014). Relapse of the disease up to 6 months after the end of initial treatment is observed in 5%–15% of cases and is usually not associated with antibiotic resistance. The most common complications of brucellosis are osteoarticular involvement, which is seen in half of patients, and others such as central nervous system involvement (10%), genitourinary involvement (5%–10%), and hepatitis (3%) (Hull and Schumaker, 2018). In endemic areas, a high percentage of patients with brucellosis are asymptomatic, and less than 10% of cases are diagnosed following early infection. The incidence of the disease in the nomadic, rural, and urban population of Hamadan province has increased from 135.4, 81.9, and 15.3 per 100,000 people in 2008 to 564.9, 168.1, and 21.8 per 100,000 population in 2013, respectively (Salari et al., 2003; Afsharpaiman and Mamishi, 2008). Also, several articles have been reported on the complications of the disease, including spondylitis, arthritis, sacroiliitis, epididymoarthritis, neurobrosulosis, cerebrovascular thrombosis, and involvement ocular from Hamadan province (Hajia et al., 2009; Keramat et al., 2009; Ranjbar et al., 2009; Eini et al., 2012; Hashemi et al., 2012; Bazzazi et al., 2013). The relapse rate of brucellosis in Hamadan province has been reported to be between 5% and 17% according to several articles (Hajia and Keramat, 2003; Ranjbar et al., 2007; Keramat et al., 2009; Hashemi et al., 2012). Because brucellosis can become chronic and recurrent, such as other chronic diseases, it needs to be registered. In addition, the main motivation for proposing this registration system is to provide the conditions for conducting other studies to respond to the prognosis of complications and relapse of disease. Due to the disabilities in patients with complications of brucellosis and the consequences of the disease, such as loss of labor, economic losses, and reduced productivity, the existence of a registration system that can monitor the occurrence of complications and recurrence of the disease and its prognosis is essential. Therefore, recording the relapse and complications of brucellosis in rural and urban areas of Hamadan province is considered a health priority in the region. To be able to have effective solutions in diagnosis, control, and prevention of complications and relapse of brucellosis in the affected population. Materials and MethodsThis qualitative registration study was conducted from September 2015 to January 2017 (the first phase of the registration program). All patients with final diagnosis of brucellosis admitted to Sina Hospital and outpatients referred from public and private medical centers to Imam Khomeini Clinic or Infectious Diseases Clinic in Sina Hospital from all cities of Hamadan province were included in the study. After obtaining written consent from the patients, all data were entered by infectious disease physicians in a questionnaire designed to register the relapse and complications of brucellosis in Hamadan province. The questionnaire consisted of four sections: demographic, signs and symptoms of disease, complications of brucellosis, and the results of paraclinical tests consisted of 73 questions. Completion of the questionnaire and clinical examination of the patient was done by infectious disease physicians. After that, the information on the questionnaires was initially reviewed by the expert, if the questionnaires were incomplete, they were reviewed and completed, and after confirming the data, they were entered into the recurrence and toll registration software. Periodic clinical examinations of patients with clinical signs with a history of brucellosis and follow-up of patients with brucellosis complications were performed every 3 months by physicians until 6 months after the completion of treatment. The design system is available at http://brucellosisregistry.umsha.ac.ir/. The software was divided into four parts including demographic information, clinical signs, disease complications, laboratory signs, and follow-up of patients in case of relapse. Complications of brucellosis were diagnosed based on International Statistical Classification of Diseases and Related Health Problems entered the software (World Health Organization, 2007). The study was approved by the Ethics Committee of Hamadan University of Medical Sciences ID: Ref: 16.35.1.4218. A brucellosis patient was defined a person who has a positive serological test [Wright greater than or equal to 1/80 or 2-mercaptoethanol greater than or equal to 1/40 or a Coombs Wright ≥ 1/80 with clinical symptoms (fever, sweating, weight loss, anorexia, muscle or bone pain compatible with brucellosis)] or positive blood culture for Brucella (Zeinali and Shirzadi, 2009). Relapse of brucellosis was defined recurrence of clinical symptoms and signs of brucellosis or brucellosis-positive blood culture from 3 months after cessation of initial treatment to a maximum of 2 years (Hull and Schumaker, 2018). Exclusion criteriaPatients who developed brucellosis for the first time and did not have any complications were excluded from the study. Complication of brucellosis was defined as involvement of any organ including the spine, meninges, heart, joints, and urogenital tract) due to Brucella with a positive Brucella serology test or blood culture or sterile fluid culture samples to diagnose brucellosis. Relapse complication was defined as concurrent relapse with involvement of any organ and a positive Brucella serology test or blood culture. Statistical analysisThe data of this study were reported using descriptive statistics indicators including tables and graphs as well as frequency and percentage. Central statistics (mean, standard deviation, mode, and range) were used to describe the continuous variables. These variables mean in two groups and more than two groups compared by T-test and analysis of variance, respectively. Categorical variables frequency were compared by chi-square test. All data were analyzed using SPSS version 16 and STATA software version 12. Statistical significance was defined as p < 0.05. ResultsIn the qualitative registration program from September 2015 to January 2017, in the first phase of the study, a total of 248 patients 155 (62.5%) male and 93 (37.5%) female with relapse or complicating brucellosis were entered and registered. The mean age of patients was 43.38 ± 17.76 years with a range of 13–92 years and the mean age in men was 42.50 ± 18.97 years and women were 44.84 ± 15.52 years. There was no significant difference in the age of patients among relapse, complication, and relapse complication groups (p=0.293). In total, out of 248 patients, 42 (16.93%, 95% CI: 12.48%, 22.19%) were in the relapse group, 154 (62.1%, 95% CI: 55.74%, 68.18%) were in the complication group and 52 (20.96%, 95% CI: 16.07%, 26.56% ) were in the relapse-complication group. The highest number of patients were men with 155 (62.5%) and also in both sexes the highest age group of patients was 21–30 years with 50 cases (20.16%). Moreover, 199 patients (80.24%) were hospitalized and 200 people (80.65%) lived in rural areas (with one nomadic residence). Among the cities, the highest number of registered cases was 84 (33.87%) patients from Hamedan city and then the cities of Kaboudar Ahang 42 (16.94) and Bahar 33 (31.13) had the most cases of registered clients, respectively. Clinical symptoms include fever, chills, weakness, fatigue, sweating, sleep disorders, weight loss, anorexia, headache, general body aches, back pain, joint pain, abdominal pain, testicular pain (men), constipation, diarrhea, cough, and behavioral disorders were evaluated in patients. The highest clinical sign of fever was observed in 203 patients (81.85%, 95% CI: 76.48%, 86.44%) of patients and the lowest behavioral disorders were observed in 14 patients (5.65%, 95% CI: 3.12%, 9.29%) of patients (Table 1). Also, clinical signs including fever, joint swelling, splenomegaly, vertebral tenderness, orchitis (in men), rash, lymphadenopathy, hepatomegaly, stiff neck, heart murmur, and jaundice were evaluated. The highest frequency of vertebral tenderness was observed in 112 patients (45.16%, 95% CI: 38.85%, 51.585), and the lowest clinical sign of heart murmur was observed in 1 patient (0.40%, 95% CI: 0.01%, 2.22%) of patients (Table 1). Table 1. Clinical manifestations of brucellosis among relapse, complications, and relapse-complication groups.
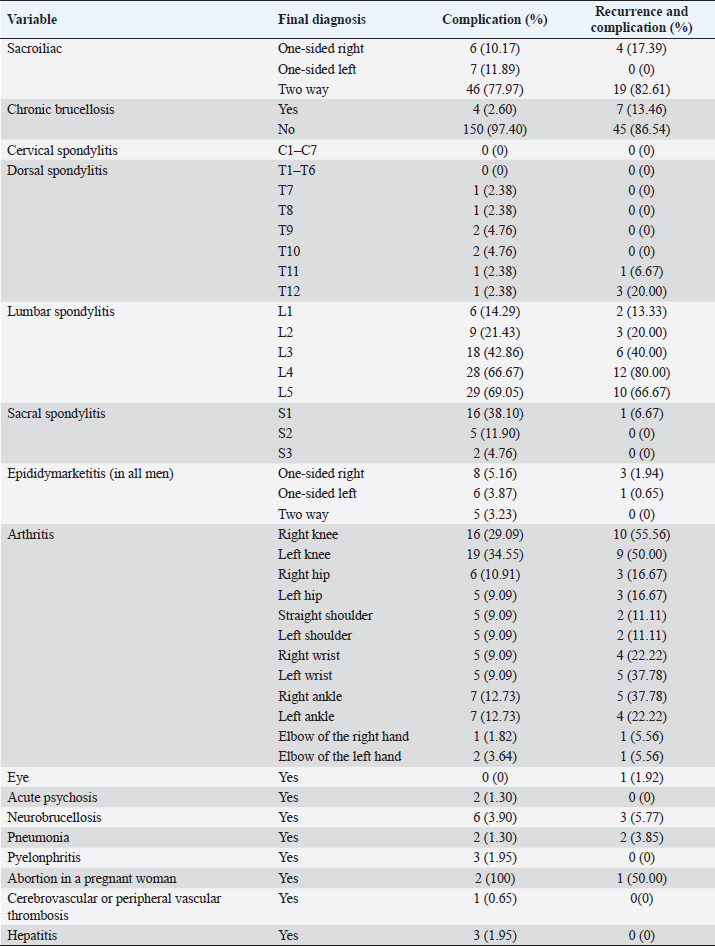
In the complication group, 81 (32.5%) men and 43 (34.68%) women were rural, and in the relapse and complication group, 7 (77.78%) men and 2 (22.22%) women were urban. Only one case of a nomadic female patient was registered in the complication group. A total of 85 patients (34.27%) were treated at the time of referral and 163 patients (65.73%) presented without a history of treatment. The duration of the disease based on the final diagnosis of brucellosis varied from a minimum of 3 days to a maximum of 365 days with an average of 56.61 days. Table 2. Comparison of organ involvements in brucellosis patients in complication, and relapse-complication groups.
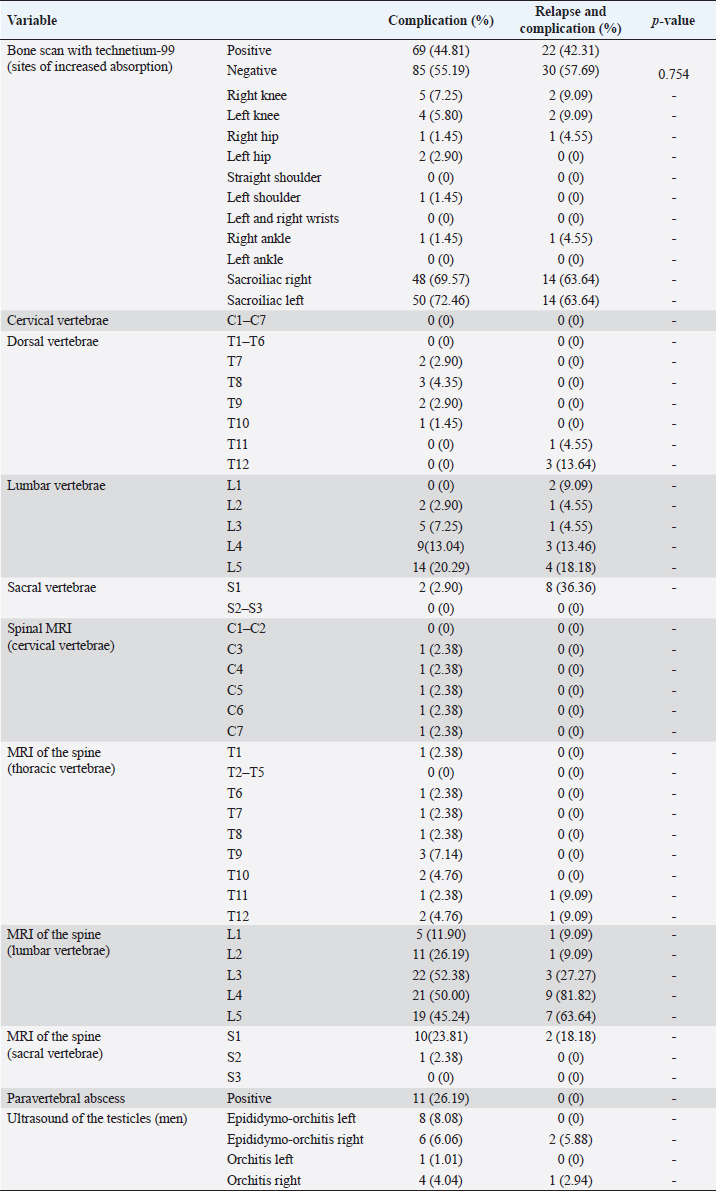
Table 3. Comparison of paraclinical findings in patients with brucellosis in relapse, complication, and relapse-complication groups.
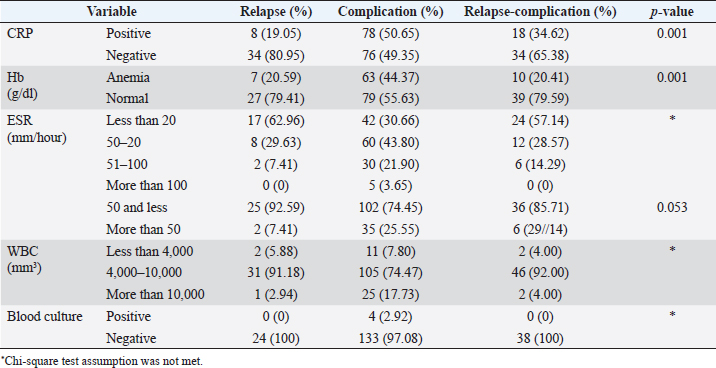
Table 4. Comparison of laboratory findings in brucellosis patients in relapse, complication, relapse-complication groups.
A total of 86 (34.68%) patients had a history of brucellosis and the rest had no history. The most common occupations were rancher, housewife, and farmer 91 (37.14%), 89 (63.33%), and 70 (28.57%), respectively. The type of contact with livestock, keeping livestock at the place of residence was the highest at 135 (83.33%), and then contact with live livestock was 109 (67.28%), and temporary contact with livestock during travel included the lowest 2 (1.23%) cases. Table 2 shows the patients with relapse or complication of brucellosis. Brucella endocarditis and abdominal abscesses (liver and spleen) were not seen in any of the patients. The most common routes of transmission in the relapse-complication group were unpasteurized milk and cheese consumption in 95 (88.79%) and 90 (84.11%) patients, respectively. Most patients had a history of consuming unpasteurized milk and cheese. In bone scan with technetium 99, the highest frequency in right and left sacroiliac was seen in 62 (68.13%, 95% CI: 57.58%, 77.51%) and 64 (70.33%, 95% CI: 59.83%, 79.45%) patients, respectively. Epididymorchitis was seen in 23 male patients (14.83%, 95% CI: 9.64%, 21.42%) (Table 3). The highest rate of anemia was seen in 63 patients (44.37%, 95% CI: 30.60%, 52.93%) in the complication patients and C-reactive protein (CRP) positive was seen in 78 patients (50.65%, 95% CI: 42.48%, 58.78%). Erythrocyte sedimentation rate (ESR) above 100 were also found in 5 patients with brucellosis. Leukopenia and leukocytosis were reported in 15 patients (6.67%, 95% CI: 3.77%, 10.75%) and 28 (12.44 CI: 8.43%, 17.48%), respectively (Table 4). DiscussionHamadan province is one of the provinces with a high incidence of brucellosis, which in 2012 and 2013 was 62.9 and 81.4 per 100,000 people, respectively. In 2014, the incidence rate in Iran was 26 cases per one 100,000 population while in Hamadan province, the incidence rate (91 per 100,000 people) was almost three times the incidence rate in the same year. The incidence of the disease in the nomadic, rural, and urban population of Hamadan province in 2013 was 564.9, 168.1, and 21.8 per 100,000 population, respectively. The brucellosis relapse and complications registration program has been launched as the first registration program in Iran to clarify the nature and frequency of complications of brucellosis and the implementation of strategies to prevent this disease. In this program, patients with acute brucellosis were not registered without relapse and complication because the goal of all brucellosis patients was not to refer but to record relapse and complications of brucellosis. No articles have been found to record relapses and complications of brucellosis. In the first phase, from September 2015 to January 2017, a total of 248 patients [155 (62.5%) male and 93 (37.5%) female] with relapse or complicating brucellosis entered the study and were registered in the designed software. The mean age of patients was 42.50 ± 18.97 years for men and 44.84 ± 15.52 years for women, and there were no significant differences in the age of patients among the relapse, complication, and relapse complication groups. A total, of 248 patients 42 (16.93%) were in the relapse group, 154 (62.1%) in the complication group, and also 52 (20.96%) in the relapse-complication group. The minimum age in men in the complication group was 13 years and women 17 years and the highest age in male patients in the complication group was 92 years old and in female patients in the relapse group was 77 years old. The highest number of patients was 62.5% men and also in both genders the highest age group of patients 30–21 years 20.16% was observed. Of 248 patients, 80.24% of them were hospitalized. In this study, 80.24% of patients were rural, one patient was nomadic, and the rest of them were urban. Among the cities, the highest number of registered cases was 33.87% from Hamadan city, and then Kaboudar Ahang and Bahar cities, had the most registered patients, respectively, and 25 patients were outside of Hamedan province. In the study by Eini et al. (2012) of 230 patients with brucellosis between 2005 and 2010 in Hamadan, 43.5% of the patients were men and the mean age of the patients was 40.84 years old which 72.2% of patients were residents of the village. The gender of the patients was different from the present study but the study of Hajia et al. (2009) reported 809 patients with brucellosis between the ages of 15 and 110 between 2000 and 2004 in Hamadan, 61.2% were men. Also the study of Hashemi et al. (2015) in Hamadan, reported that 149 patients in the age range of 11–82 years, 70.47% of male patients were consistent with our study. In the present study, the highest incidence rate of brucellosis was in the complication group 62.1%. The duration of the disease based on the final diagnosis of brucellosis ranged from a minimum of 3 days to a maximum of 365 days with an average of 56.61 days, and also 34.68% of patients had a medical history of brucellosis. In this study, the occupations of ranchers, housewives, and farmers were 37.14%, 63.33%, and 28.57%, respectively. In addition, the history of contact with livestock such as keeping livestock in the place of residence was 83.33%, and then contact with live animals was 67.28%. In the present study, the most common clinical manifestation was fever in 81.85% of patients. Also, vertebral tenderness was 45.16%, and a heart murmur was observed in one patient. In the study of Hajia et al. (2009) conducted in Hamadan, the most common clinical signs and symptoms were fever (83.8%), arthralgia (80.34%), chills (63.1%), anorexia (59.45%), and fatigue (51.9%), respectively. In another study by Eini et al. (2012), the most common signs and symptoms were fever (77.4%), arthralgia (70%), sweating (46.9%), fatigue (46.5%), and back pain (45.7%). Both of the above studies were similar to our study; however, in the studies of Keramat et al. (2009) and Hashemi et al. (2012) arthralgia and fatigue were the most common clinical symptoms which were different from the present study. The main reason is that in the present study, patients with acute brucellosis for the first time without complications were not registered. In the present study, 14.83% of male patients had epididymorchitis, which was consistent with other studies conducted in Hamadan (Keramat et al., 2009; Eini et al., 2012; Hashemi et al., 2015). Also in this study, complicating brucellosis were seen such as neurobrocellosis at 3.63%, pyelonephritis at 1.21%, chronic brucellosis at 4.84%, ocular involvement in one patient (0.40%) and hepatitis in three patients (1.21%). Three (75%) of four pregnant women had abortions; however, endocarditis and abdominal abscesses (liver and spleen) were of the registered patients. In addition, most patients had a history of consumption of unpasteurized milk 88.79%, and cheese 84.11%. in the relapse and complication group. The study by Eini et al. (2012) reported that the most common route of transmission was consumption of contaminated dairy products (60.3%). In the present study, in whole-body bone scan with technetium 99, the most common involvement was seen in right and left sacroiliacs in 68.13% and 70.33% of patients, respectively. In the study of Hashemi et al. (2015) on 149 patients with brucellosis, sacroiliitis in 45% and spondylitis in 30.2% were reported. In this study, there were 9 patients (3.63%) with neurobrosulosis, which is more than the study of Ranjbar et al. (2009) in 2009, among 1,375 patients with brucellosis who were hospitalized in the infectious ward of Sina Hospital in Hamadan between 2001 to 2005, 20 patients (1.45%) reported a final diagnosis of neurobrocellosis including 12 men and 8 women. In a study by Haj-Abdolbaqi et al. (2008) at Imam Khomeini Hospital in Tehran between 1990 to 2004, 31 patients with a diagnosis of neurobrucellosis reported that 61% of patients were men and the study by Pourhassan (2007) 43 patients with neurobrocellosis between 1996 to 2005 in Tabriz, 28 (58%) of patients were men which both were similar to our study. In this study, one patient had cerebrovascular thrombosis and three patients had acute brucellar hepatitis. The studies of Keramat and Hashemi (2015) and Keramat and Torkaman Asadi (2014) reported two patients with brucellar hepatitis and one case of right internal jugular vein thrombosis with acute complicated brucellosis. Eye involvement is a rare complication that was one case (0.4%) in this study. In a 2008 study by Bazazi et al. (2013) at Sina Hospital in Hamadan, a 29-year-old man with acute brucellosis reported bilateral optic neuritis and retinal hemorrhage after treatment, all symptoms of the disease disappeared and had a complete recovery, and no recurrence was observed in 12 months of follow-up. In a study by Hashemi et al. (2012) between 2008 and 2010 in Hamadan comparing the three-drug regimens of doxycycline-streptomycin (DS), doxycycline-rifampin (DR), and ofloxacin-rifampin (OR), the relapse rate at the end of 6 months of clinical follow-up with the regimen DS4 6.4% with DR diet 15.3% and OR diet 7.8% have been reported. In a study by Ranjbar et al. (2007) on 228 patients with brucellosis between 1999 and 2001 in Hamadan, two DR treatment regimens were compared with DR-amikacin the relapse rate in the 6-month follow-up of patients with two-drug regimen was 9.3% and with three-drug regimen was 5.7%. However, in the study of Hajia and Keramat (2003) which she performed on 542 brucellosis patients in Hamadan between 1994 to 1999, the relapse rate during the 2 years of follow-up was 36 cases (6.64%). All the last three studies had different relapse rates from the present study, because we enrolled and registered all cases with clinical forms of relapse and/or complication in this registry, and the patient with primary acute brucellosis without complications was excluded, as it was not one of the goals of the registration program. Laboratory findings include normal white blood cell count, leukopenia, lymphocytosis, anemia, thrombocytopenia, elevated liver function tests, and elevated ESR were reported in different studies (Zeinali and Shirzadi, 2009; Olsen and Palmer, 2014; Franc et al., 2018; Hull and Schumaker, 2018). In the present study, anemia was seen in 35.56% of patients, with the highest rate of relapse in patients with relapse and complication group 44.37% and the highest rate of CRP positive in the group of patients with complication 50.65%. Elevated ESR more than 50 was observed in 20.87% of patients and ESR above 100 was observed in 5 patients with complicated brucellosis. Leukopenia and leukocytosis were observed in 6.67% and 12.44% of patients, respectively. However, in a study by Hashemi et al. (2007) on 245 brucellosis patients (152 men and 93 women) with a mean age of 26.9 years, in Hamadan. Anemia, leukocytosis, and ESR above 30 mm/hour were observed in 5.2%, 44.9%, and 39.6% of brucellosis patients with osteoarticular complications, respectively. In the present study, anemia was higher but leukocytosis was lower this may have been due to the high relapse and complications of brucellosis patients. In another study conducted by Eini et al. (2012) between 2005 and 2010 at Sina Hospital in Hamadan anemia, leukocytosis, ESR above 30 mm/hour, and positive CRP were observed in 14.8%, 20.8%, 59.5%, and 52.9% of patients, respectively. Also, in a study by Torkamanasadi et al. (2017) among 149 brucellosis patients in Hamadan, anemia, leukocytosis, positive CRP, and elevated ESR were reported in 36.9%, 17.4%, 87.9%, and 53.7%, respectively, which the percentage of anemia and leukocytosis and elevated ESR and positive CRP are almost similar to the present study. The limitations of our study were included: a patient with acute brucellosis for the first time without complication was excluded and all brucellosis patients during the time frame of the research were not accepted for registration or they did not come to visit because of their personal reasons or long distance of residence from different cities of the province. ConclusionBased on the results and access to this information can be used in the process of diagnosis and care of patients with relapse and complications of brucellosis. Therefore, the results of this study can be used for evidence-based decision-making to diagnose and better manage complications in patients with brucellosis. AcknowledgmentsThe authors would like to thank Dr. Maryam Adabi, Dr. Hossein Erfani, Dr. Jalaledin Amiri, Dr. Rashid Heidari Moghadam, Dr. Mohammad Reza Ebadian, MR. Seyed Jalal Batahi, Dr. Peyman Eini, and Dr. Mohammad Mahdi Majzoobi who helped us in the implementation of this project and the authors would also like to express their sincere gratitude to Mr.Mojtaba Mohammadian for designing a software program for the registration of relapse and complications of brucellosis. Also, they would like to acknowledge the Deputy Minister of Research and Technology of the Ministry of Health and Medical Education for financial support, and the Vice Chancellor for Research and Technology of Hamadan University of Medical Sciences is sincerely grateful for the financial support and launching of the registration program on the website of Hamadan University of Medical Sciences in the form of a research plan with the approved number 9408054218 dated 2015-10-27. ReferencesAfsharpaiman, S. and Mamishi, S. 2008. Brucellosis: review of clinical and laboratory features and therapeutic regimens in 44 children. Acta Med. Iran. 46, 489–494. Bazzazi, N., Yavarikia, A. and Keramat, F. 2013. Ocular involvement of brucellosis. Middle East Afr. J. Ophthalmol. 20(1), 95–97. Eini, P., Keramat, F. and Hasanzadeh Hoseinabadi, M. 2012. Epidemiologic, clinical and laboratory findings of patients with brucellosis in Hamadan, west of Iran. J. Res. Health Sci. 12(2), 105–108. Franc, K.A., Krecek, R.C., Häsler, B.N. and Arenas-Gamboa, A.M. 2018. Brucellosis remains a neglected disease in the developing world: a call for interdisciplinary action. BMC Public Health 18(1), 125; doi:10.1186/s12889-017-5016-y. PMID: 29325516; PMCID: PMC5765637. Haji-Abdolbagi, M., Rasooli-Nejad, M., Jafari, S., Hasibi, M. and Soudbakhsh, A. 2008. Clinical and laboratory findings in neurobrucellosis: review of 31 cases. Arch. Iran Med. 11(1), 21–25. Hajia, M. and Keramat, F. 2003. Study on the rate of brucellosis relapse & efficiency different protocols in among hospitalized patient in educational hospital of Hamadan. J. Mil. Med. 5(3), 195–199. Hajia, M., Rahbar, M. and Keramat, F. 2009. Epidemiological, clinical, diagnostic and treatment aspects of hospitalized brucellosis patients in Hamadan. Ann. Trop. Med. Public Health 2, 42–45. Hashemi, S.H., Gachkar, L., Keramat, F., Mamani, M., Hajilooi, M., Janbakhsh, A., Majzoobi, M.M. and Mahjub, H. 2012. Comparison of doxycycline–streptomycin, doxycycline–rifampin, and ofloxacin–rifampin in the treatment of brucellosis: a randomized clinical trial. Int. J. Infect. Dis. 16(4), e247–e251. Hashemi, S.H., Keramat, F., Ranjbar, M., Mamani, M., Farzam, A. and Jamal-Omidi, S. 2007. Osteoarticular complications of brucellosis in Hamadan, an endemic area in the west of Iran. Int. J. Infect. Dis. 11(6), 496–500. Hashemi, S.H., Torkaman Asadi, F., Alikhani, M.Y. and Naseri, Z. 2015. Comparison of culture and erological methods for the diagnosis of brucellosis. Sci. J. Hamadan Univ. Med. Sci. 22(1), 37–42. Hull, N.C. and Schumaker, B.A. 2018. Comparisons of brucellosis between human and veterinary medicine. Infect. Ecol. Epidemiol. 8(1), 1500846; doi:10.1080/20008686.2018.1500846. PMID: 30083304; PMCID: PMC6063340. Keramat, F. and Hashemi, S.H. 2015. Acute brucellar hepatitis: report of two cases. Avicenna J. Clin. Microb. Infect. 2(2), e23908; doi:10.17795/ajcmi-23908 Keramat, F., and Torkaman Asadi, F. 2014. A case report of right internal jugular vein thrombosis with acute brucellosis. Sci. J. Hamadan Univ. Med. Sci. 21(2), 161–166. Keramat, F., Ranjbar, M., Mamani, M., Hashemi, S.H. and Zeraati, F. 2009. A comparative trial of three therapeutic regimens: ciprofloxacin-rifampin, ciprofloxacin-doxycycline and doxycycline-rifampin in the treatment of brucellosis. Trop. Doct. 39(4), 207–210. Olsen, S.C. and Palmer, M.V. 2014. Advancement of knowledge of Brucella over the past 50 years. Vet. Pathol. 51(6), 1076–1089; doi:10.1177/0300985814540545. Epub 2014 Jun 30. PMID: 24981716. Pourhassan, A. 2007. Clinical and laboratory findings in neurobrucellosis: a study of 43 cases. Iran. J. Clin. Infect. Dis. 2(2), 71–76. Ranjbar, M., Keramat, F., Mamani, M., Kia, A.R., Hashemi, S.H. and Nojomi, M. 2007. Comparison between doxycycline–rifampin–amikacin and doxycycline–rifampin in the treatment of brucellosis. Int. J. Infect. Dis. 11(2), 152–156. Ranjbar, M., Rezaiee, A.A., Hashemi, S.H. and Mehdipour, S. 2009. Neurobrucellosis: report of a rare disease in 20 Iranian patients referred to a tertiary hospital. East. Mediterr. Health J. 15(1), 143–148. Salari, M.H., Khalili, M.B. and Hassanpour, G.R. 2003. Selected epidemiological features of human brucellosis in Yazd, Islamic Republic of Iran: 1993-1998. Eastern Mediterr. Health J. 9, 1054–1060. Torkaman Asadi, F.T., Hashemi, S.H., Alikhani, M.Y., Moghimbeigi, A. and Naseri, Z. 2017. Clinical and diagnostic aspects of brucellosis and antimicrobial susceptibility of Brucella isolates in Hamedan, Iran. Jpn. J. Infect. Dis. 7, 235–238; doi:10.7883/yoken.JJID.2016.133 World Health Organization. 2007. International statistical classification of diseases and related health problems (ICD-10), 10th revision. Geneva, Swtizerland: WHO Publications. Zeinali, M. and Shirzadi, M.R. 2009. National guideline for brucellosis control. Tehran, Iran: Ministery of Health and Medical Education, pp: 12–35. | ||
| How to Cite this Article |
| Pubmed Style Keramat F, Karami M, Mamani M, Saadatmand A, Hashemi SH, Alikhani MY, Bashirian S, Shivapour Z. Relapse and complications of brucellosis: Findings of a disease quality registry. J Microbiol Infect Dis. 2023; 13(3): 155-164. doi:10.5455/JMID.2023.v13.i3.8 Web Style Keramat F, Karami M, Mamani M, Saadatmand A, Hashemi SH, Alikhani MY, Bashirian S, Shivapour Z. Relapse and complications of brucellosis: Findings of a disease quality registry. https://www.jmidonline.org/?mno=302657423 [Access: January 25, 2026]. doi:10.5455/JMID.2023.v13.i3.8 AMA (American Medical Association) Style Keramat F, Karami M, Mamani M, Saadatmand A, Hashemi SH, Alikhani MY, Bashirian S, Shivapour Z. Relapse and complications of brucellosis: Findings of a disease quality registry. J Microbiol Infect Dis. 2023; 13(3): 155-164. doi:10.5455/JMID.2023.v13.i3.8 Vancouver/ICMJE Style Keramat F, Karami M, Mamani M, Saadatmand A, Hashemi SH, Alikhani MY, Bashirian S, Shivapour Z. Relapse and complications of brucellosis: Findings of a disease quality registry. J Microbiol Infect Dis. (2023), [cited January 25, 2026]; 13(3): 155-164. doi:10.5455/JMID.2023.v13.i3.8 Harvard Style Keramat, F., Karami, . M., Mamani, . M., Saadatmand, . A., Hashemi, . S. H., Alikhani, . M. Y., Bashirian, . S. & Shivapour, . Z. (2023) Relapse and complications of brucellosis: Findings of a disease quality registry. J Microbiol Infect Dis, 13 (3), 155-164. doi:10.5455/JMID.2023.v13.i3.8 Turabian Style Keramat, Fariba, Manochehr Karami, Mojgan Mamani, Ali Saadatmand, Seyyed Hamid Hashemi, Mohammad Yousef Alikhani, Saeid Bashirian, and Zahra Shivapour. 2023. Relapse and complications of brucellosis: Findings of a disease quality registry. Journal of Microbiology and Infectious Diseases, 13 (3), 155-164. doi:10.5455/JMID.2023.v13.i3.8 Chicago Style Keramat, Fariba, Manochehr Karami, Mojgan Mamani, Ali Saadatmand, Seyyed Hamid Hashemi, Mohammad Yousef Alikhani, Saeid Bashirian, and Zahra Shivapour. "Relapse and complications of brucellosis: Findings of a disease quality registry." Journal of Microbiology and Infectious Diseases 13 (2023), 155-164. doi:10.5455/JMID.2023.v13.i3.8 MLA (The Modern Language Association) Style Keramat, Fariba, Manochehr Karami, Mojgan Mamani, Ali Saadatmand, Seyyed Hamid Hashemi, Mohammad Yousef Alikhani, Saeid Bashirian, and Zahra Shivapour. "Relapse and complications of brucellosis: Findings of a disease quality registry." Journal of Microbiology and Infectious Diseases 13.3 (2023), 155-164. Print. doi:10.5455/JMID.2023.v13.i3.8 APA (American Psychological Association) Style Keramat, F., Karami, . M., Mamani, . M., Saadatmand, . A., Hashemi, . S. H., Alikhani, . M. Y., Bashirian, . S. & Shivapour, . Z. (2023) Relapse and complications of brucellosis: Findings of a disease quality registry. Journal of Microbiology and Infectious Diseases, 13 (3), 155-164. doi:10.5455/JMID.2023.v13.i3.8 |